CASE OF THE WEEK – “Monostotic Fibrous Dysplasia of Left Tibia” by Dr ShekharShikare, HOD & Consultant, Nuclear Medicine & Dr. Milind Raje, Consultant Radiology, NMC Royal Hospital Sharjah
Monostotic Fibrous Dysplasia of Left Tibia
The Incremental Value of Radionuclide Bone Scintigraphy in Fibrous Dysplasia of Bone
Introduction
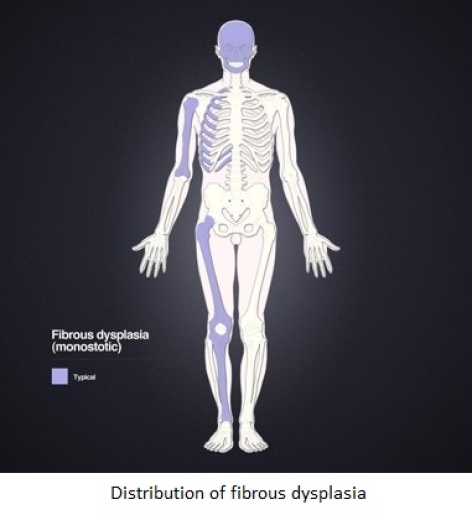
The term fibrous dysplasia (FD) was coined by Lichtenstein in 1938 to describe a subset of benign bone tumors manifesting in childhood or early adult life. FD has a tendency of predominantly unilateral involvement and a prolonged clinical course characterized by pain, deformity, and pathologic fracture of the affected bones. FD can be manifested as a single lesion (monostotic) or as multiple lesions (polyostotic). According to Ippolito and colleagues, in monostotic FD, the most commonly appearing site is on the femur. Tibia, humerus, rib, clavicle and craniofacial skeleton are the next in order of frequency. McCune-Albright syndrome is known as a combined condition consisting of polyostotic bone involvement, precocious puberty, hyperthyroidism and café au lait cutaneous macules. Mazabraud syndrome is associated with single or multiple intramuscular myxomas in monostotic or polyostotic form.
It can be evaluated by conventional radiography, scintigraphy, magnetic resonance imaging and Computed Tomography Scans (CT) although CT is considered the exam of choice in the evaluation of craniofacial lesions.
Case
A 24-years old gentleman with history of pain in left leg and limping since last few months. No history of any trauma, sports, fever etc.
Computed tomography of legs
It shows a solitary lesion, which eccentrically located in lower 1/3rd of left tibial shaft with expansion and thinning of the cortical outline and ground glass density of the marrow. It has sharp zone of demarcation from adjacent normal bone. No cortical discontinuity or periosteal reaction or soft tissue component associated with it favors monostotic fibrous dysplasia left tibial shaft (figure 1,2 & 3)
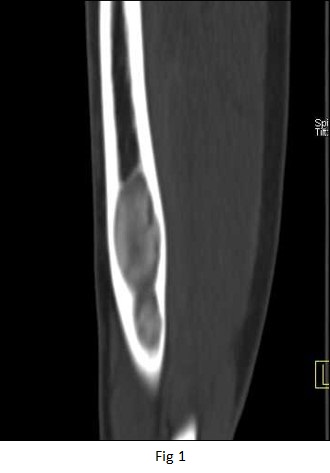

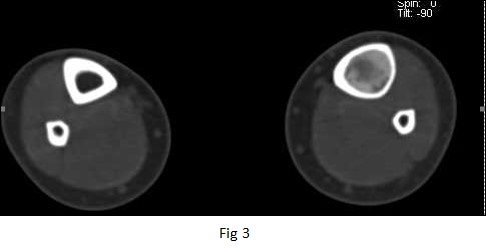
Figure 1,2 & 3 - CT Scan images of the left tibia
Referred for 99mTc MDP whole body bone and SPECT CT scintigraphy to evaluate if it is MONOSTOTIC or POLYSTOTIC fibrous dysplasia.
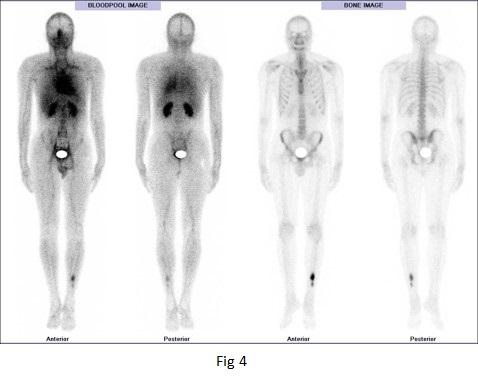
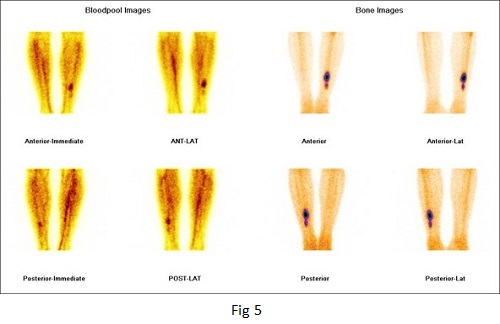
Figure 4 & 5 - 99mTc MDP whole body bone and spot images of the legs.
Two phase bone scintigram (Blood pool & delayed bone images shown here) demonstrates a hot spot in the left tibia caused by increased uptake of the radioisotope tracer technetium-99m methylene diphosphonate (99m Tc MDP). The increased uptake is already visible in the early blood pool phase confirms that involvement is confined to the lower 1/3rd of shaft left tibia, without evidence of disseminated disease (monostotic)
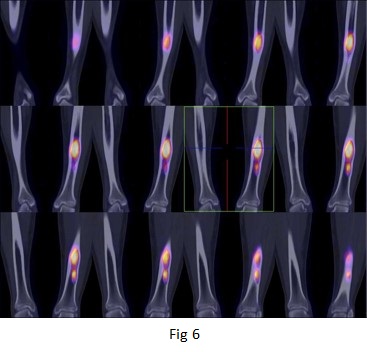
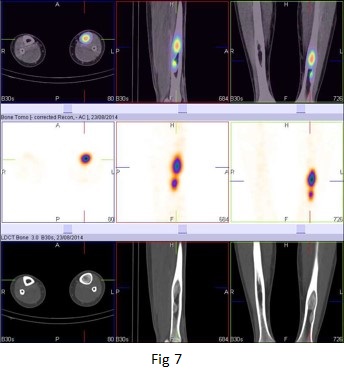
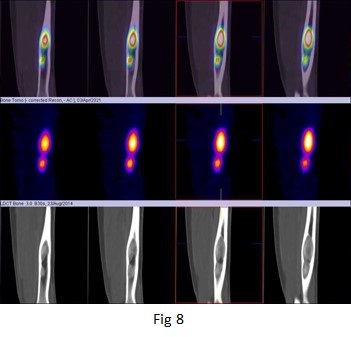
Figure 6,7 & 8 - 99mTc MDP bone SPECT CT fused images of the left tibia.
There is intense focal area (approximately fusiform shaped) of increased tracer uptakes in 1/3rd shaft left tibia.
Discussion
FD is considered a common, benign skeletal disorder. Single-bone lesions of monostotic presentation without any other disturbance are the most common forms of FD, and monostotic FDs are known to enlarge in proportion to skeletal growth. Polyostotic forms are less common and often continue to enlarge after complete skeletal maturation. This feature can cause progressive deformity and increased prevalence of pathologic fractures in polyostotic FD. The most common skeletal deformity in FD is a discrepancy between the lengths of bilateral limbs, referred to as shepherd’s crook deformity of the proximal part of the femur.
Clinically, several imaging modalities are used routinely. In simple radiographs, FD presents as a well-marginated peripheral sclerotic bone lesion with a variety of patterns, which may be lucent, sclerotic, or mixed or may have a ground glass appearance, depending on the amount of bone trabeculae, fibrous elements and calcification. Endosteal scalloping and focal cortical thinning may be present without cortical disruption or periosteal reaction. Computed tomography, which is often required, accurately delineates the extent of skeletal involvement and may be useful in evaluating craniofacial FD or lesions suspected to be sarcomatous transformations.
During scintigraphy studies, FD typically exhibits markedly increased radionuclide accumulation in both early perfusion and delayed bone imaging. Even at low specificity, increased uptake in a delayed view is sensitive for early detection and assessment of the extent of involvement.
Radionuclide bone scans are of certain value in the diagnosis of FD and useful in determining the extent of the skeletal involvement especially in polyostotic lesions. The diagnostic specificity of FD with radionuclide bone scanning can be improved in association with other imaging modalities such as X-rays. CT scan with contrast, SPECT-CT enhances sensitivity for lesions detection over planar bone scintigraphy. In addition to improve anatomic localization of scintigraphy findings, this equipment offers the opportunity to add true diagnostic information derived from CT imaging.
Literature stated the diagnosis is generally clear after a proper radiological and scintigraphy workup. However, biopsy might be needed if the diagnosis is doubtful or malignant transformation is suspected.



