CASE OF THE WEEK – “Parathyroid Adenoma without Hyperparathyroidism” by Dr ShekharShikare, HOD & Consultant, Nuclear Medicine NMC Royal Hospital Sharjah
Introduction
In general, parathyroid tumors are classified into adenoma, hyperplasia, cystic changes, and carcinoma. The differentiation between adenoma and hyperplasia is often difficult in usual histopathological examinations. Compared to hyperplasia, parathyroid adenomas often present a higher increase in the level of serum parathyroid hormone (PTH). Bone fractures, calculi of the urinary tract and higher serum calcium levels are more frequently the first symptoms of parathyroid adenomas than of hyperplasia’s. This case report presents a rare case of PTH producing parathyroid adenoma with normal levels of serum PTH and calcium.
Case
29 years old gentleman with history of right sided neck swelling with some pressure symptoms such as shortness of breath and swallowing difficulties since last one month.
Biochemistry
PTH 61.5 pg /mL (15-68.3), Sr calcium 2.40 mmol/L (2.10-2.60).
Sr Creatinine 0.47 mg/dL (0.5-1.2), Sr uric acid 2.9 mg/dl (3.5-7.2),TSH 0.992 microIU/ml (0.270- 4.2)
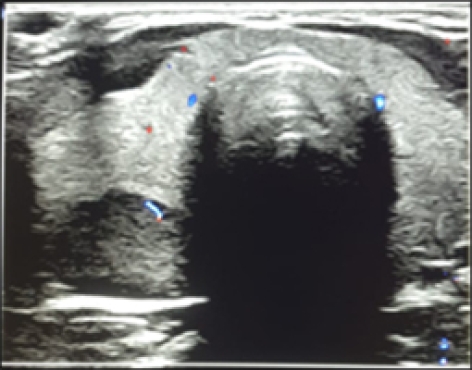
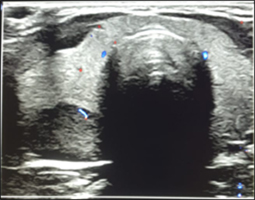
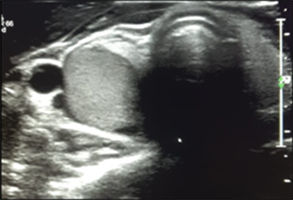
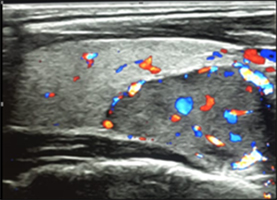
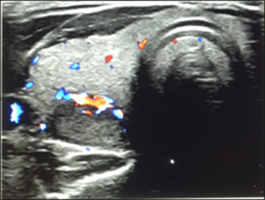
Ultrasound Neck
Well defined hypoechoic nodule with halo and cystic changes 3.15*1.82 CMS in the posterior peripheral region of lower pole showing vascularity on color doppler and looks indenting right lobe suggesting right parathyroid adenoma
(figure 1 to 5)

Ref for 99mTcSESTAMIBI PARATHYROID SCINTIGRAPHY
99mTc-MIBI PARATHYROID IMAGES
EARLY AND DELAYED MIBI IMAGES OF NECK AND CHEST
It shows focal area of increased MIBI tracer uptakes (approximately 1.7*2.0 cms in size) seen infero-posterior portion of the right lobe of thyroid gland on early images. (Better appreciated in SPECT-CT fused images) and shows mild persistent tracer retention in the same region on delayed washout images (Better appreciated in SPECT-CT fused images figure 7 to 9).
99mTc-THYROID IMAGES
The right lobe measures 4.5*2.7 cms in size and left lobe 3.8*2.0 cms in size approximately. Area of reduced tracer uptakes seen in infero-lateral portion of the right lobe (possibly to be due to underlying lesion as described above). Rest of the gland shows good tracer uptakes.
Conclusion- The Possibility Of Metabolically Active Parathyroid Adenoma (1.7*2.0 Cms Approximately In Size) Infero-Posterior Portion To The Right Lobe of Thyroid Gland Without Hyperparathyroidism.
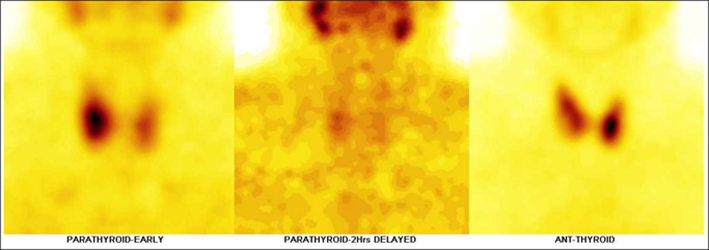
Figure 6
99mTc-Sestamibi parathyroid & 99mTc- thyroid static images
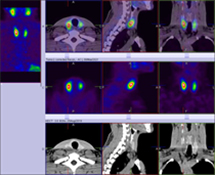
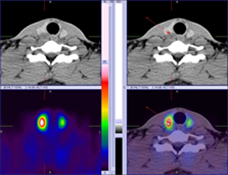
99mTc-Sestamibi parathyroid Hybrid SPECT CT images shows metabolically active parathyroid adenoma (1.7*2.0 cms in size) infero-posterior portion of the right lobe of thyroid gland.
Subsequently patient underwent surgical removal of the tumor and Immunohistology confirmed that there was proliferation of chief cells with positive parathyroid hormone (PTH) staining. Thus, the tumor was diagnosed as parathyroid adenoma despite a lack of clinical evidence for hyperparathyroidism. The reason for the lack of clinical features of hyperparathyroidism in this adenoma still remains unclear, however, there might be inactivation of hormone excretion, possibly due to insufficiency of blood supply. This was a very rare case of parathyroid adenoma exhibiting no clinical evidence of hyperparathyroidism.
Discussion
Most parathyroid adenomas are functional and manifest hypercalcemia causing bone fractures and urinary tract calculi. The parathyroid tumor in the current case displayed a medullary growth of adenomatous tissue of the parathyroid chief cells. There were small cystic changes and hemorrhages within the tumor, but necrosis was not observed. The tumor was considered to have arisen in one of the right parathyroid glands. The remaining parathyroid adenoma on the right side probably became atrophic because of the expanding nature of the tumor. There were two normal-sized parathyroid glands on the left side, which led to the diagnosis of parathyroid adenoma rather than hyperplasia. In the current case, levels of serum PTH, calcium was normal despite the positive PTH immuno-staining of the tumor cells.
We think that such a case is extremely rare because nearly all parathyroid adenomas reported have been functional with an increased level of serum PTH and manifestations of hyperparathyroidism. There were reported cases of ‘norm calcemic hyperparathyroidism’, in which renal calculi and hypercalciuria were present while the serum levels of total calcium and intact PTH were normal, and the serum ionized calcium level was elevated. Parathyroid adenomas were present in some of the cases reported as norm calcemic hyperparathyroidism. The present case was different from those previously reported as norm calcemic hyperparathyroidism because there were no manifestations such as urinary tract calculi or hypercalciuria.
There would be two possible reasons for having a non-functioning parathyroid adenoma with positive PTH staining in the current case: either a low level of PTH production or inhibition of the release of the hormone into the bloodstream. However, the exact mechanism for the non-functional nature of the parathyroid adenoma was not apparent in the current case. There were no glandular cells in the wall of the cystic part of the lesion, which might be a reason for not having the hormone secreted into the bloodstream. However, the mechanism of formation for the solid part of the lesion remained unclear. The measurement of intact PTH in the blood of both left and right middle thyroid arteries might allow the differentiation between functioning and non-functioning adenoma of the parathyroid gland.



